
News
Nearly 200 Harvard Affiliates Rally on Widener Steps To Protest Arrest of Columbia Student

News
CPS Will Increase Staffing At Schools Receiving Kennedy-Longfellow Students

News
‘Feels Like Christmas’: Freshmen Revel in Annual Housing Day Festivities

News
Susan Wolf Delivers 2025 Mala Soloman Kamm Lecture in Ethics

News
Harvard Law School Students Pass Referendum Urging University To Divest From Israel
Boston Doctors Lead the Medical Unionization Wave
After more than a year of negotiations over their first contract, residents at Mass General Brigham sensed growing momentum for a strike in January.
Such a decision, made by 2,700 doctors working at the state’s largest private employer, would have major ramifications for the healthcare industry. While strikes at health care practices are rare — and require days’ notice — they have also become more frequent in recent years.
But for MGB Housestaff United, a Boston-area medical union formed in 2023 under the Committee of Interns and Residents, a local of the Service Employees International Union, President Donald Trump’s inauguration — and subsequent decision to fire two high-ranking officials at the National Labor Relations Board — forced them to reconsider.
“Going on strike or putting forward any kind of unfair labor practices in front of a more pro-employer NLRB could put our union and other unions that are more in the private sector across the country at risk,” said Love W. Osunnuga, a first-year MGB resident and union bargaining committee member.
The union’s decisons about what to accept in their final contract, and whether a strike remains truly off the table, will set new precedent for union efforts that have sprouted since MGB Housestaff United was recognized two years ago.
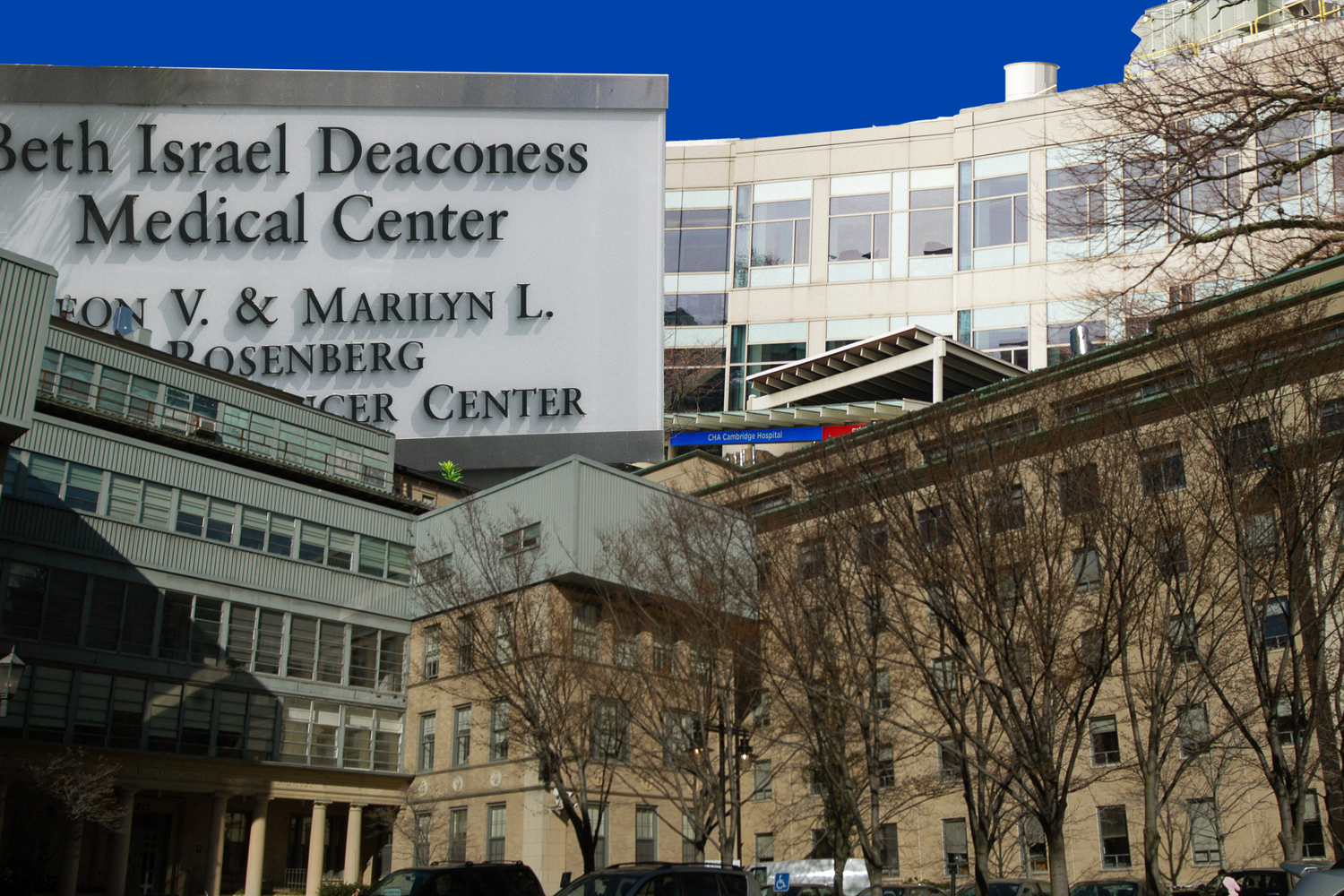
Since June 2023, when residents at MGB first voted to unionize, at least five other medical union efforts have begun for residents, physicians, and nurses at Boston-area hospitals. In 2025 alone, clinicians at the Cambridge Health Alliance, a public employer, voted to unionize — as did residents and fellows at Beth Israel Deaconess Medical Center.
Boston is not the only city experiencing a wave of medical unionization.
From 2000 to 2022, only 2 percent of all union petitions in the U.S. were filed for attending physicians. But in the last two years, physicians’ unions have made up 23 percent of all petitions, even as the number of election petitions has also skyrocketed.
And the number of workers represented by the CIR-SEIU — which represents medical interns, residents, and fellows across the country — has doubled from 2021 to 2024.
The unions cover different kinds of medical labor, formed in both public and private workplaces. But concerns over working conditions and autonomy, exacerbated by the Covid-19 pandemic, lie at the crux of the movement.
John August, a healthcare specialist at Cornell University’s School of Industrial and Labor Relations, said that the growth in organizing over the past few years has “caught the industry off guard.”
“I think we’re in a period of new struggle here that MGB is a good example of,” he said.
‘We’re Still Catching Up’
The Covid-19 pandemic catalyzed organizing efforts across the medical field. As hospitals operated at full capacity, staff members struggled to keep up with the inflow of patients.
Psychologist Drew E. Madore said that when he joined the Cambridge Health Alliance in June 2021, doctors were left scrambling to complete administrative duties because the hospital had assumed a certain number of no-shows.
Osunnuga also said that staff shortages at MGB’s Brigham and Women’s Faulkner Hospital during the pandemic were a serious concern.
“Sometimes you would need a stat lab for someone that you were really concerned about, maybe you thought they were having a heart attack, and you wanted to get a troponin draw, but you couldn’t find a phlebotomist to even do it,” she said.
These concerns spurred residents’ and fellows’ unionization efforts at MGB in 2023, as workers demanded greater autonomy and access to resources such as personal protective equipment.
“Covid really exposed a lot of the vulnerabilities that residents and just healthcare personnel in general face around workplace safety and just our general working conditions,” Sascha N. Murillo, then a third-year resident at MGB, said in 2023.
During the pandemic, the desire to win wage increases to compensate for record inflation — hitting almost 9 percent in June 2022 — also drove unionization. In Boston and Cambridge, residents are often forced to live in areas with especially high cost of living close to the hospitals.
Though pandemic-era inflation has largely subsided, physicians say they are still dealing with the fallout.
“Five years later, it feels like we’re still catching up and just everybody is much sicker now and needs a lot more support,” CHA family doctor Jeremy C. Stricsek said. “I think it takes much more time and emotional effort to provide quality care for our patients.”
‘No Leverage’
The latest group of workers to unionize — attending physicians — have been influenced by a shift away from private practice in the last decade, as well as growing corporatization of the field, according to August.
In Cambridge, the first group of attending physicians to unionize were joined by psychologists and physician associates in a State Healthcare and Research Employees unionization effort at Cambridge Health Alliance. But across the country, at least a dozen attending physician unions have already been recognized.
While physicians that completed their residency have historically held their own individual or group private practices, they have increasingly become employees of hospitals and hospital-owned practices in recent years. In the last decade, the share of private-practice physicians dropped from 60 percent to 47 percent.
August said this shift has come with a loss in agency.
“They really have no leverage in that relationship other than the fact that they’re doctors and the hospital needs them,” he said. “They’re not really in a position to negotiate as they were when they were private practitioners.”
Stricsek said the August closure of two Steward Health Care hospitals — acquired by a private equity firm in 2010 — has also caused an influx of new patients for Cambridge Health Alliance hospitals.
“Thankfully, we don’t have private equity running us into the ground, but because private equity has done that elsewhere, that’s affecting our patient volume, and again, that their ability to provide care to people,” Stricsek said.
MGB, in particular, has seen major growth in its acquisitions of community hospitals over the past 30 years, acquiring seven hospitals and medical centers since 1996.
The result, according to physicians across Boston hospitals, has been an emphasis on efficiency at the expense of physicians’ autonomy.
“It’s treating both doctors and patients like numbers, as if we are just working on an assembly line and we’re just supposed to churn out as much productivity as possible,” Madore said.
CHA primary care physician Emily R. Chen said that residents and fellows’ unionization efforts have been fueled by “regular life needs,” including rent, reasonable work hours, and medical-school debt.
CHA spokesperson David Cecere wrote in an emailed statement that the hospital system is “constantly working to support the engagement and well-being of all of our staff and providers.”
“We offer various supports for our staff and providers to address burnout, which is a major issue in health care across the nation,” he wrote. “Because the needs of our communities are significant, especially for mental health and primary care services, we are always working to increase our patients’ access to care.”
‘Unprecedented’
In the Boston area, organizing has been taking place most visibly within MGB, BIDMC, and CHA.
“There’s just been a tremendous level of organizing in the last five years,” August said. “Unprecedented, just unprecedented.”
Experts said recent organizing in the medical sphere has been bolstered by union gains in other fields. According to labor expert and Harvard Law School professor Benjamin I. Sachs, recent years have seen the rise of unions comprising mostly younger workers — including graduate students and academic workers.
But the Trump administration’s actions to curb the power of the NLRB have given both unionized student-workers and residents cause for concern.
The Harvard Graduate Students Union-United Auto Workers and the MGB residents and fellows both withdrew unfair labor practice charges in advance of Trump’s inauguration, citing concerns about the future of the board. Organizers are particularly concerned that the board might use the charges to reverse the 2016 Columbia University decision guaranteeing graduate students’ right to unionize.
And because residents and fellows are not fully board certified and are trained by attending physicians, their status as employees has also been contentious before. Only two decades ago, in 1999, the NLRB ruled that residents were employees for the purposes of unionizing — a decision which could be reversed under the Trump administration.
Even if the board is able to meet a quorum, August said cases on contentious labor law rulings, including the classification of student-workers as employees, could be reversed.
“I think we’re going to see an attack on union security,” he said. “I think we’re going to have some cases go to the Supreme Court, and the Supreme Court’s in a position to make the National Labor Relations Act unconstitutional. Do I think that’s going to happen? I think there’s a chance it might.”
At MGB, according to third-year neurology resident and bargaining committee member Alexander M. Cerjanic, the union is planning a new wave of actions ahead of Match Week, when medical students are matched to hospitals where they will complete their residencies.
“If we don’t use our voices to make sure that resources are at the point of care and where they need to be, we’re going to talk about the challenges that we face and really try to educate the public to bring them along in this fight,” Cerjanic said.
—Staff writer Hugo C. Chiasson can be reached at hugo.chiasson@thecrimson.com. Follow him on X @HugoChiassonn.
—Staff writer Amann S. Mahajan can be reached at amann.mahajan@thecrimson.com. Follow her on X @amannmahajan.
Want to keep up with breaking news? Subscribe to our email newsletter.
Most Read
From Our Advertisers

Over 300+ courses at prestigious colleges and universities in the US and UK are at your disposal.

With innovative financial tools combined with financial education, Collegiate empowers students to take control of their finances and build confidence in their money management skills.

Serve as a proctor for Harvard Summer School (HSS) students, either in the Secondary School Program (SSP), General Program (GP), or Pre-College Program.

With an increasingly competitive Law School admissions process, it's important to understand what makes an applicant stand out.
Welcome to your one-stop gifting destination for men and women—it's like your neighborhood holiday shop, but way cooler.

Admit Expert is a premium MBA admissions consulting company, helping candidates secure admission to top B-schools across the globe with significant scholarships.
